Some cases of acute leukemia are composed entirely of undifferentiated-appearing blasts. These cases are difficult (or impossible) to diagnose morphologically (under the microscope) – you really need special tests like immunophenotyping in order to make a definitive diagnosis.
Other cases of acute leukemia have obvious morphologic clues. Acute promyelocytic leukemia (APL) falls into the latter category. It is composed of malignant promyelocytes, which often have a distinctive appearance.
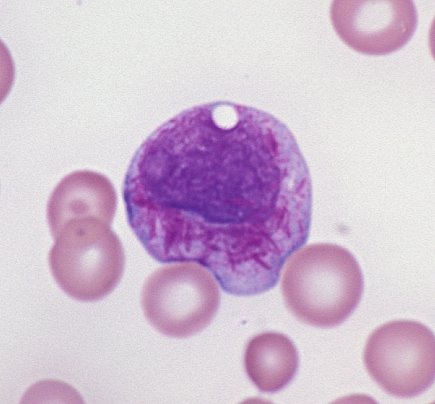
But the really characteristic finding in APL is the faggot cell, so named because it contains a ton of Auer rods all piled up on each other, resembling a bundle of sticks (or faggot). When you see these, you can make the diagnosis of APL based on morphology alone, without waiting for molecular or cytogenetic studies (which will show the characteristic t(15;17) of APL – but which take some time to perform).
Making an immediate, morphologic diagnosis is critical in cases of APL, because these patients cannot be given routine acute myeloid leukemia chemotherapeutic agents. The malignant promyelocytes of APL contain lots of granules which have strong procoagulant activity. If you give the patient typical acute leukemia treatment, the promyelocytes will burst, the nasty granules will be released, and the patient will be at high risk for disseminated intravascular coagulation (DIC), a very dangerous syndrome in which patients bleed and clot all over the body.
Fortunately, there is a drug called all-trans retinoic acid (or ATRA) that works great for patients with APL because it causes the malignant promyelocytes to mature (into myelocytes, then metamyelocytes, then neutrophils). Then the patient can be treated with regular chemotherapy without risk of DIC.







I know the word “faggot” has different meanings, such as a bag of sticks or cigarettes (“fag”), but I think a name change for the “faggot cell” wouldn’t be completely uncalled for. Maybe I’m being to PC on this, but just imagine trying to explain to a patient “Yeah, you’ve got a build up of these faggot cells.”
“What did you call me??”
I couldn’t agree more. I feel the need to explain the term to my students, some of whom may not be aware of the original meaning. Maybe we could find out who first described the cells and use that person’s name as a descriptor.
Very nice image and description of AML. I must say that Auer rod was first described by Thomas McCrae in 1905 and later by John Auer in 1906. Promyelocytes containing at least 10 Auer rods are referred to as “faggot” cells. However, such a designation is more artificial.